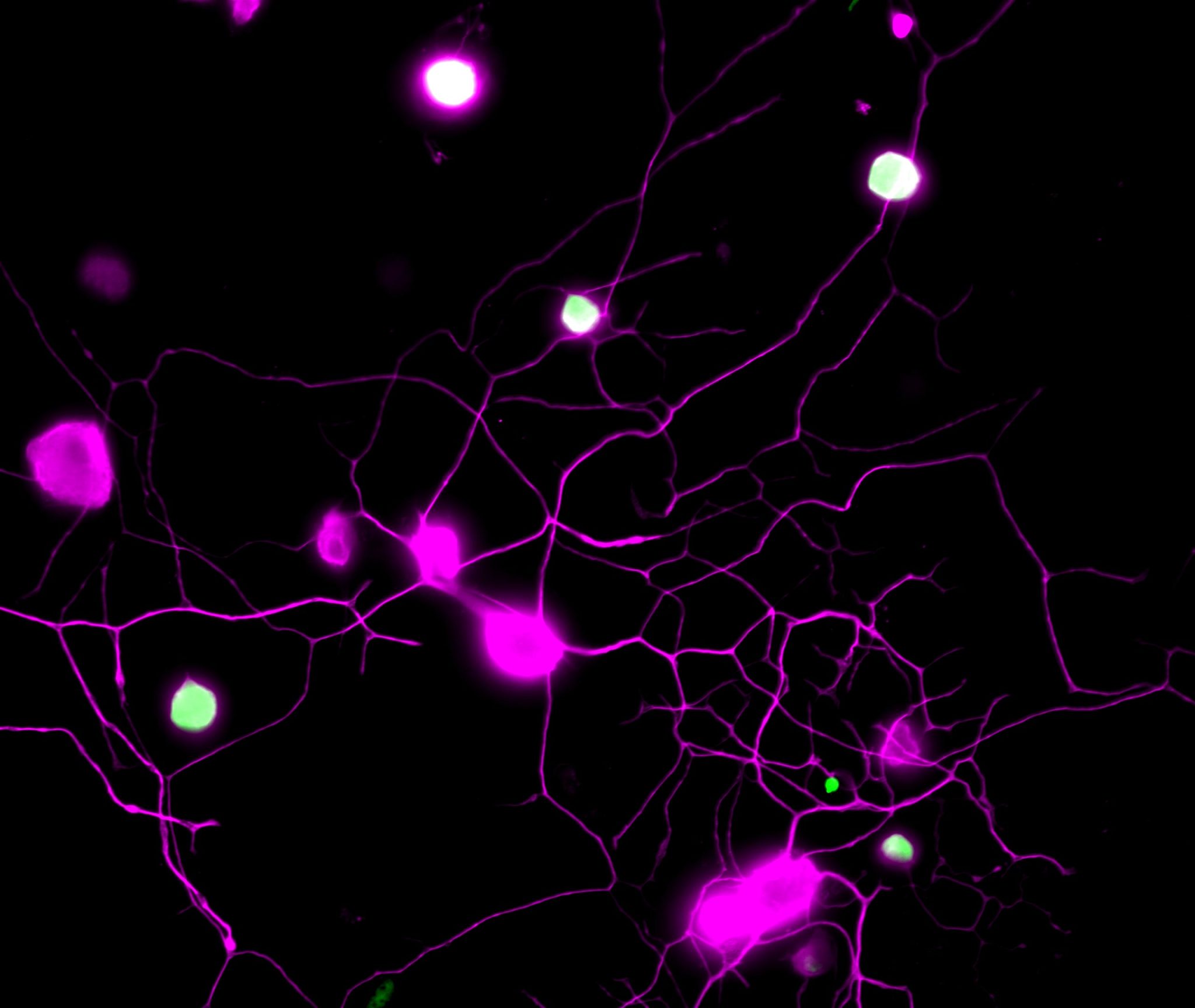
Mouse sensory neurons are proven in magenta. BH4, the molecule driving continual ache, is proven in inexperienced. Therefore, the neurons “in ache” are seen in inexperienced/white. Credit score: ©Cronin/IMBA
Recent hope for ache administration from newly recognized hyperlink between continual ache and lung most cancers in mice.
Though it's uncomfortable, ache is a crucial alarm system that alerts us to tissue injury and prompts us to withdraw from dangerous conditions. Though ache is predicted to subside as accidents heal, many sufferers expertise persistent ache lengthy after restoration. Now, a brand new examine factors to attainable new therapies for continual ache with a shocking hyperlink to lung most cancers. The work, which was printed in Science Translational Drugs, was spearheaded by a world workforce of researchers at IMBA – Institute of Molecular Biotechnology of the Austrian Academy of Sciences, Harvard Medical College, and Boston Youngsters’s Hospital. Their findings of the analysis, carried out in laboratory mouse fashions, open up a number of therapeutic alternatives that would enable the world to enhance continual ache administration and curtail the opioid epidemic.
Acute ache is a crucial hazard sign. Alternatively, continual ache relies on persistent damage and might even be skilled within the absence of a stimulus, damage, or illness. Although tons of of tens of millions of persons are affected, continual ache is among the many least well-managed areas of healthcare. To enhance how persistent ache is managed, particularly in mild of the raging opioid disaster, it's paramount to develop novel medication based mostly on a basic understanding of the underlying mechanisms.
“We had beforehand proven that sensory neurons produce a selected metabolite, BH4, which then drives continual ache, reminiscent of neuropathic ache or inflammatory ache,” says challenge lead and co-corresponding creator Shane Cronin. He's a employees scientist within the Penninger lab at IMBA and a former postdoc within the Woolf lab at Harvard Medical College and F.M. Kirby Neurobiology Middle, Boston Youngsters’s Hospital. “The concentrations of BH4 correlated very properly with the ache depth. So, we naturally thought that this was an important pathway to focus on.”
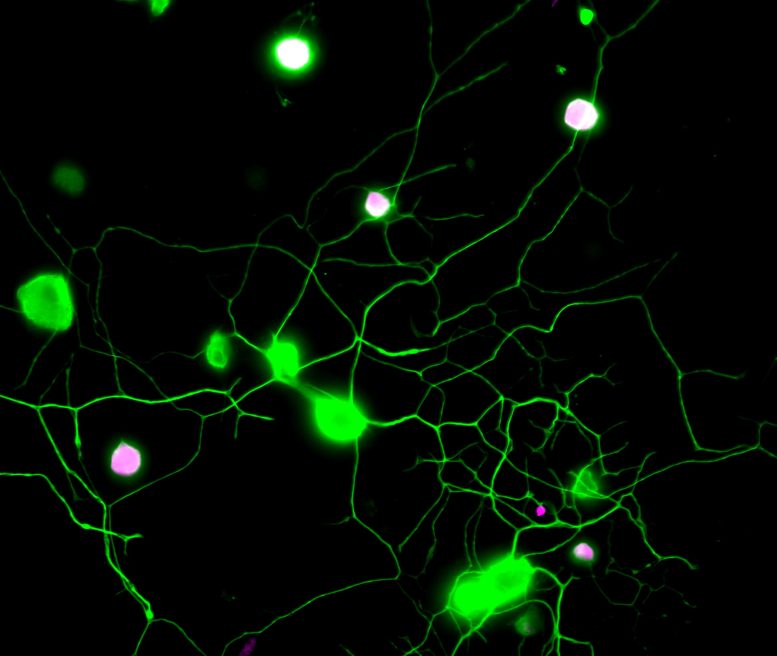
Mouse sensory neurons are proven in inexperienced. BH4, the molecule driving continual ache, is proven in magenta. Therefore, the neurons “in ache” are seen in magenta/white. Credit score: ©Cronin/IMBA
To determine medication that cut back BH4 ranges in ache neurons, the scientists carried out a “phenotypic display” of 1000 target-annotated, FDA-approved drugs. This method allowed the researchers to begin their search utilizing drugs which are at the moment in use for numerous indications, and to determine undescribed, off-target analgesic properties. Among the many preliminary findings of this hypothesis-driven search, the workforce was capable of hyperlink the beforehand noticed analgesic results of a number of medication, together with clonidine and capsaicin, to the BH4 pathway. (Clonidine is a prescription treatment sometimes used to decrease blood stress and capsaicin is the lively element of chili peppers.)
“Nonetheless, our phenotypic display additionally allowed us to ‘repurpose’ a shocking drug,” says Cronin. The drug ‘fluphenazine’, which is an antipsychotic that has been used to deal with schizophrenia. “We discovered that fluphenazine blocks the BH4 pathway in injured nerves. We additionally demonstrated its results in continual ache following nerve damage in vivo.” The scientists additionally discovered that the efficient analgesic dose of fluphenazine of their experiments within the mouse mannequin is similar to the low finish of the doses safely indicated for schizophrenia in people.
Moreover, the display uncovered a novel and surprising molecular hyperlink between the BH4 pathway and EGFR/KRAS signaling, a pathway concerned in a number of cancers. Blocking EGFR/KRAS signaling lowered ache sensitivity by reducing the degrees of BH4. The genes of EGFR and KRAS are the 2 most ceaselessly mutated genes in lung most cancers, which prompted the researchers to take a look at BH4 in lung most cancers. Surprisingly, by deleting an vital enzyme, GCH1, within the BH4 pathway, the mouse fashions of KRAS-driven lung most cancers developed fewer tumors and survived for much longer. Therefore, the analysis workforce uncovered a standard signaling pathway for continual ache and lung most cancers by means of EGFR/KRAS and BH4, thus opening up new avenues of therapy for each situations.
“Power ache is at the moment subjected to usually ineffective palliative therapies. Moreover, efficient painkillers reminiscent of opioids can lead, if used inappropriately, to extreme habit. It's subsequently vital to search out and develop new and repurposed medication to deal with continual ache,” says co-corresponding creator Clifford Woolf, professor of neurology and neurobiology at Harvard Medical College and director of the F.M. Kirby Neurobiology Middle at Boston Youngsters’s Hospital.
One intriguing side of the examine is the mechanistic hyperlink between ache and lung most cancers. “The identical triggers that drive tumor progress seem like additionally concerned in setting the trail to continual ache, usually skilled by most cancers sufferers. We additionally know that sensory nerves can drive most cancers, which may clarify the vicious circuit of most cancers and ache,” provides co-corresponding creator Josef Penninger. He's an IMBA group chief and founding director, who's at the moment additionally the director of the Life Sciences Institute on the College of British Columbia (UBC), Vancouver, Canada. “Understanding these cross-talks is subsequently not solely vital for most cancers therapies however may also assist to enhance the standard of life for most cancers sufferers in the direction of much less ache.”
Reference: “Phenotypic drug display uncovers the metabolic GCH1/BH4 pathway as key regulator of EGFR/KRAS-mediated neuropathic ache and lung most cancers” by Cronin, S. J. F., et al., 31 August 2022, Science Translational Drugs.
DOI: 10.1126/scitranslmed.abj1531
Funding: Harvard Medical College, Austrian Federal Ministry of Schooling, Science and Analysis, Austrian Academy of Sciences, Metropolis of Vienna, Austrian Science Fund, T. von Zastrow basis, a Canada 150 Analysis Chairs Program, Canadian Institutes of Well being Analysis, Harvard Stem Cell Institute, NIH/Nationwide Institutes of Well being
Post a Comment