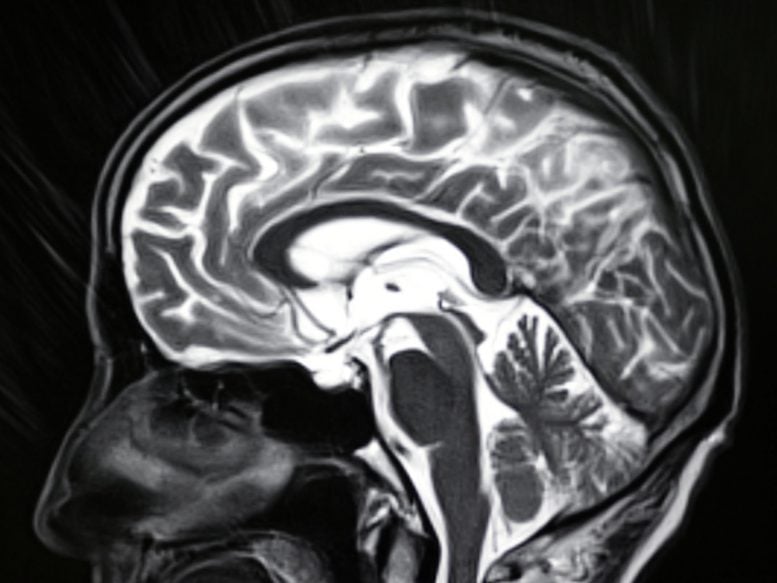
Human mind MRI picture.
The mind construction of sufferers with current onset psychosis and melancholy can supply essential organic insights into these diseases and the way they may develop.
In a brand new research revealed right now (April 12, 2022) in Organic Psychiatry, researchers on the College of Birmingham present that by analyzing structural MRI scans of the mind, it’s attainable to establish sufferers most inclined to poor outcomes.
By figuring out these sufferers within the early phases of their sickness, clinicians will have the ability to supply extra focused and efficient therapies.
“At present, the way in which we diagnose most psychological well being issues relies on a affected person’s historical past, signs, and scientific observations, fairly than on organic data,” says lead creator Paris Alexandros Lalousis. “Meaning sufferers might need comparable underlying organic mechanisms of their sickness, however totally different diagnoses. By understanding these mechanisms extra absolutely, we may give clinicians higher instruments to make use of in planning therapies.”
Within the research, the researchers used knowledge from round 300 sufferers with current onset psychosis and up to date onset melancholy collaborating within the PRONIA research. PRONIA is a European Union-funded cohort research investigating prognostic instruments for psychoses which is going down throughout seven European analysis facilities together with Birmingham.
The researchers used a machine studying algorithm to evaluate knowledge from sufferers’ mind scans and type these into teams, or clusters. Two clusters have been recognized based mostly on the scans, every of which contained each sufferers with psychosis and sufferers with melancholy. Every cluster revealed distinctive traits which associated strongly to their chance of restoration.
Within the first cluster, decrease volumes of gray matter – the darker tissue contained in the mind concerned in muscle management and features comparable to reminiscence, feelings, and decision-making – have been related to sufferers who went on to have poorer outcomes. Within the second group, in distinction, increased ranges of gray matter signaled sufferers who have been extra more likely to get well properly from their sickness.
A second algorithm was then used to foretell the sufferers’ situation 9 months following the preliminary analysis. The researchers discovered a better degree of accuracy in predicting outcomes when utilizing the biologically based mostly clusters in comparison with conventional diagnostic techniques.
Proof additionally confirmed that sufferers within the cluster with decrease volumes of gray matter of their mind scans could have increased ranges of irritation, poorer focus, and different cognitive impairments beforehand related to melancholy and schizophrenia.
Lastly, the staff examined the clusters in different massive cohort research in Germany and the US and have been in a position to present that the identical recognized clusters could possibly be used to foretell affected person outcomes.
“Whereas the PRONIA research contained individuals who have been lately identified with their sickness, the opposite datasets we used contained folks with persistent situations,” explains Lalousis. “We discovered that the longer the period of sickness, the extra doubtless it was that a affected person would match into the primary cluster with decrease gray matter quantity. That actually provides to the proof that structural MRI scans might be able to supply helpful diagnostic data to assist information focused therapy choices.”
The following step for the staff is to begin to validate the clusters within the clinic, gathering affected person knowledge in actual time, earlier than planning bigger scale scientific trials.
Reference: “Neurobiologically Primarily based Stratification of Latest Onset Melancholy and Psychosis: Identification of Two Distinct Transdiagnostic Phenotypes” by Paris Alexandros Lalousis, MSc; Lianne Schmaal, PhD; Stephen J. Wooden, PhD; Renate L.E.P. Reniers, PhD; Nicholas M. Barnes, PhD; Katharine Chisholm, PhD; Sian Lowri Griffiths, PhD; Alexandra Stainton, PhD; Junhao Wen, PhD; Gyujoon Hwang, PhD; Christos Davatzikos, PhD; Julian Wenzel, MSc; Lana Kambeitz-Ilankovic, PhD; Christina Andreou, MD; Carolina Bonivento, PhD; Udo Dannlowski, MD; Adele Ferro, PhD; Theresa Liechtenstein, MD; Anita Riecher-Rössler, MD; Georg Romer, MD; Marlene Rosen, PhD; Alessandro Bertolino, MD; Stefan Borgwardt, MD; Paolo Brambilla, MD; Joseph Kambeitz, MD; Rebekka Lencer, MD, PhD; Christos Pantelis, MB BS, MD, MRCPsych, FRANZCP; Stephan Ruhrmann, MD; Raimo Okay.R. Salokangas, MD, MSc, PhD, PsD; Frauke Schultze-Lutter, PhD; André Schmidt, PhD; Eva Meisenzahl, MD; Nikolaos Koutsouleris, MD; Dominic Dwyer, PhD; Rachel Upthegrove, MBBS FRCPsych, PhD and for thePRONIA Consortium, 12 April 2022, Organic Psychiatry.
DOI: 10.1016/j.biopsych.2022.03.021
Post a Comment